Adding Someone to your health insurance is a meaningful way to provide them with essential medical coverage and peace of mind. Whether you’re looking to cover a spouse, child, or other eligible family member, including them in your health plan can give them access to preventive care, regular check-ups, and emergency support when needed. However, the process can feel complex with various eligibility requirements, documentation needs, and enrollment periods. This guide walks you through every step, from confirming who qualifies and gathering necessary paperwork to understanding potential cost changes and enrollment deadlines. “Follow these steps to confidently navigate the process and ensure your loved ones have coverage when they need it most. If you’re interested in becoming a health teacher, then”

What Is A Dependent? Understanding Health Insurance Terms
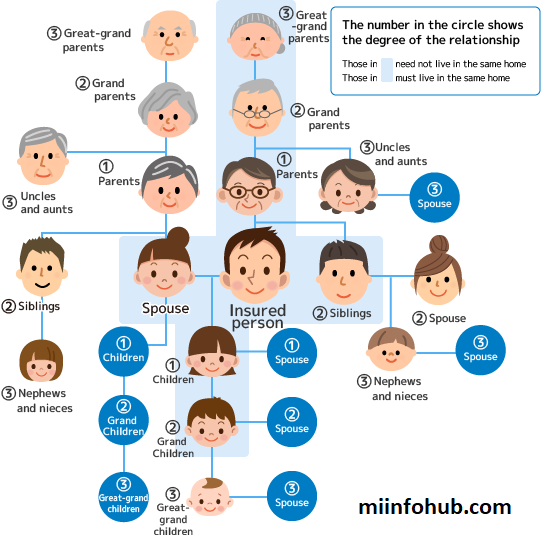
In health insurance, a “dependent” refers to someone you can add to your plan due to your relationship with them.
- Spouses or legally recognized domestic partners
- Children, including biological, adopted, or stepchildren
- Parents or other family members, in some cases
Types Of Health Insurance Plans That Allow Dependents
Different types of health insurance plans may have unique rules for dependent coverage:
- HMO (Health Maintenance Organization): Dependents must use in-network providers, limiting choices for covered care.
- PPO (Preferred Provider Organization): Offers more flexibility, allowing dependents to see both in-network and out-of-network providers.
- EPO (Exclusive Provider Organization): Requires using a specific network, though it may allow for emergency out-of-network care.
Know When You Can Add Dependents
You can typically add dependents to your health insurance during specific periods:
- Open Enrollment Period: Most changes to your plan, including adding dependents, are allowed during this annual window.
- Qualifying Life Events (QLEs): Certain life changes, known as QLEs, trigger a “Special Enrollment Period” where you can update your coverage. Common QLEs include:
- Marriage or domestic partnership registration
- Birth, adoption, or foster placement of a child
- Divorce or legal separation
- Loss of other health coverage for the dependent

Gather Required Documentation To Add Someone To Your Health Insurance
Adding a dependent requires specific documents to verify their eligibility. Be prepared to provide:
- Marriage Certificate for adding a spouse
- Birth Certificate for a newborn or dependent child
- Adoption Papers if adding an adopted child
- Proof of Relationship (like a shared address) for domestic partners
Submit The Application
The application process varies based on the insurance provider:
- Online Portal: Many providers allow dependents to be added online.
- Customer Service Call: Call the insurer directly if you need assistance.
- Employer-Provided Plans: If your insurance is through work, contact your HR department to complete the necessary paperwork.
- Forms and Information: Complete all required forms accurately to avoid delays.
Check For Any Additional Costs
Adding a dependent may increase your monthly premium. When considering costs:
- Ask about family coverage rates or dependent add-on costs.
- Compare the costs of individual vs. family plans if your employer offers multiple health plans.
- Make sure your dependent’s primary care and specific treatments are fully covered, as some policies may have limitations.
Special Enrollment Period (SEP) Scenarios
Certain events outside the regular open enrollment period allow you to make changes to your insurance. Known as Special Enrollment Periods (SEPs), these include:
- Moving to a new state where your current plan doesn’t apply
- Losing other health coverage, such as job-based or Medicaid coverage
- Death of a spouse or dependent, which impacts your household coverage
Quick Reference: Adding A Dependent To Your Health Insurance
| Dependent Type | Eligibility Requirements | Required Documentation | Enrollment Period |
|---|---|---|---|
| Spouse | Legally married or domestic partnership (where applicable) | Marriage Certificate, ID | Open Enrollment or QLE |
| Child | Biological, adopted, or stepchild under age limit | Birth Certificate, Adoption Papers | Open Enrollment or QLE |
| Domestic Partner | Registered domestic partnership (varies by insurer) | Proof of Partnership, Shared Residence Proof | Open Enrollment or QLE |
| Parent/Other Family | Eligibility varies by state and insurance plan | Proof of Relationship, Residency Verification | Open Enrollment or Special Plan Options |
Common Mistakes To Avoid When Adding A Dependent
Adding a dependent can be straightforward, but here are some common mistakes to avoid:
- Missing Enrollment Deadlines: You may have to wait until the next enrollment period if deadlines are missed.
- Incorrect Documentation: Incorrect or incomplete documents can delay coverage.
- Not Updating Marital or Household Status: Changes in household status (like divorce) need to be reported, as they can impact eligibility.
Financial Implications Of Adding A Dependent To Health Insurance
Adding a dependent usually increases your premium. Here’s how to manage potential cost increases:
- Compare Family Plan Costs: Family plans might be more cost-effective than adding individual coverage.
- Deductible and Out-of-Pocket Costs: Understand how adding a dependent affects these amounts.
- Tax Benefits: Some dependents may qualify you for tax benefits, which could offset added costs.
Wait For Confirmation
After submitting your application, it typically takes about 1-3 weeks to process. Your insurance provider will:
- Send Confirmation: Look for an email or mailed notice confirming your dependent’s addition.
- Temporary ID Cards: Some insurers issue temporary cards for new dependents until official ones are sent.
Review Policy Changes
Adding a dependent can change your overall coverage. Important areas to review include:
- Deductibles and Out-of-Pocket Maximums: Adding dependents may impact these amounts.
- Coverage Limits and Networks: Verify any limitations in coverage to avoid unexpected charges.
- Provider Availability: Make sure your dependent’s preferred providers are in-network to minimize costs.
What To Do If Coverage Is Denied
If the application is denied:
- Review the Reason for Denial: This information is usually in the denial notice.
- Appeal the Decision: Contact your insurer for appeal options, as many providers allow you to challenge decisions.
- Explore Alternative Options: Look into state or government programs like Medicaid if traditional options aren’t available.
How To Remove A Dependent If Needed
In certain situations, such as a divorce or a child aging out, you may need to remove a dependent from your policy:
- Notify Your Insurer Promptly: Failing to update changes can lead to coverage issues or penalties.
- Check for Special Provisions: Some policies may allow temporary continuation of coverage for certain dependents.
- Update Contact Information: Keep records updated to ensure correct billing and communication.

FAQs: Common Questions On Adding Dependents
Can I add a dependent if they already have insurance?
- Yes, but this may make your insurance secondary.
What if my insurance doesn’t cover domestic partners?
- Some states or insurers don’t recognize domestic partners. Look into other options if needed.
What happens if I miss the enrollment period?
- You may have to wait until the next open enrollment or a Qualifying Life Event.
Summary
Adding someone to your health insurance can be straightforward with the right knowledge. Each step, from understanding eligibility to managing financial impacts, ensures your dependent’s healthcare needs are met.


