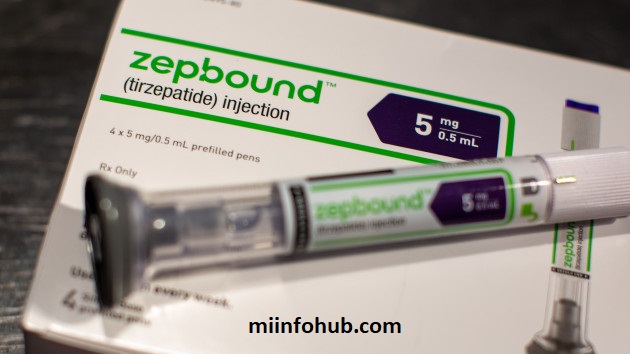
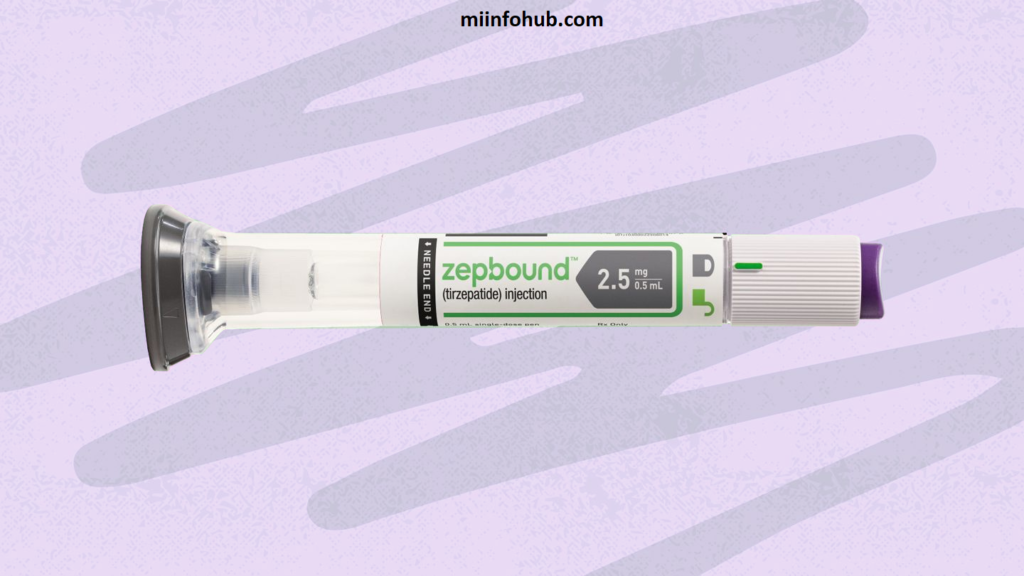
Zepbound, a newly developed medication for specific health conditions, has gained attention for its effectiveness and targeted approach. However, its high cost has many individuals wondering what health insurance covers Zepbound. This guide provides an in-depth look at how health insurance covers Zepbound, the types of plans that may provide coverage, and steps you can take to verify and maximize your benefits.

Overview Of Zepbound
Doctors prescribe Zepbound to treat specific medical conditions that require specialized medication. Due to its benefits, it has become highly sought after. However, it can be costly, making insurance coverage an important consideration for many patients. If you want to discover about what happens to health insurance when you leave a job then click here.
Health Insurance Coverage For Zepbound
Coverage for Zepbound varies widely, depending on your insurance provider, plan type, and specific policy details. Here’s how it generally breaks down:
- Employer-Sponsored Health Insurance: Some employer-based plans cover Zepbound, but coverage often depends on the specific details of your employer’s policy.
- Medicare and Medicaid: These government-funded programs may cover Zepbound, though eligibility and coverage criteria vary. Medicare Part D, for example, may cover prescription drugs, including Zepbound, depending on the plan.
- Marketplace Health Plans: Plans obtained through the Health Insurance Marketplace may cover Zepbound, though coverage depends on your specific plan tier and formulary.
- Private Health Insurance: Private insurance plans may cover Zepbound if deemed medically necessary. Confirming coverage specifics with your provider is essential.
Who Is Eligible For Zepbound Coverage?
Insurance coverage for Zepbound often depends on certain eligibility criteria, which may vary by insurance provider. Some common eligibility factors include:
- Medical necessity and doctor’s prescription
- Prior approval from the insurance company
- Meeting any specific health criteria associated with Zepbound’s prescribed conditions
How Does Zepbound Coverage Work Across Different Insurance Providers?
Insurance providers categorize medications by tiers, with Zepbound often placed in a higher, specialty drug tier. This affects both coverage and cost. The following plan types may handle Zepbound coverage differently:
- Preferred Provider Organizations (PPOs): Typically offer broader options but may have higher copays for specialty drugs.
- Health Maintenance Organizations (HMOs): Often require in-network pharmacies and prior authorizations.
- Point of Service Plans (POS): Provide flexibility but often require referrals for specialty medications like Zepbound.
Zepbound Coverage: Comparing Different Health Insurance Plans
Here’s a comparative column highlighting different health insurance aspects for Zepbound coverage, focusing on coverage types, eligibility, costs, and copayment options:
| Aspect | Private Insurance | Medicare | Medicaid | Employer-Sponsored Plans |
|---|---|---|---|---|
| Coverage Availability | Often covered but varies by plan | May be covered under Part D (prescription) if medically necessary | Coverage depends on state-specific guidelines for prescriptions | Coverage depends on the employer’s health plan |
| Eligibility | Generally available to insured members | Available to those 65+ or with qualifying disabilities | Available to low-income individuals and families, varies by state | Available to employees and sometimes dependents |
| Cost/Co-pay | May have co-pays or deductibles based on plan tier | Out-of-pocket costs if not fully covered, may include co-pays | Generally low to no cost but varies | Typically has co-pays or a portion covered by employer |
| Pre-Authorization Needed | Often required | Required for certain Part D medications | Varies by state and medication approval | Depends on employer’s policy, may require prior authorization |
| Alternative Options | Patient assistance programs may apply | Secondary insurance or Part D supplement options | State-funded assistance programs might help | May have secondary coverage options through supplemental insurance |

Steps To Verify Zepbound Coverage
To confirm if your health insurance covers Zepbound, take the following steps:
- Check Your Plan’s Formulary: Insurance plans list covered medications in a formulary. Reviewing this list will show if Zepbound is included.
- Contact Your Insurance Provider: Speak directly with your provider to understand Zepbound’s coverage, potential restrictions, and any required authorizations.
- Ask About Prior Authorization: Some plans require a prior authorization for Zepbound, meaning the insurer must approve the medication before covering it.
- Inquire About Tier Levels: Zepbound may fall under a higher-cost specialty tier, impacting copayments and coinsurance. Understanding the tier level helps you anticipate out-of-pocket costs.

Tips For Successfully Navigating Zepbound Coverage
Navigating insurance coverage for a high-cost medication like Zepbound can be complex. Here are some tips to help:
- Work Closely with Your Healthcare Provider: They can provide supporting documentation if prior authorization is required.
- Track Out-of-Pocket Costs: Keeping track of expenses helps you meet any deductible quickly.
- Understand Your Plan’s Appeal Process: If coverage is initially denied, consider appealing with your provider’s support.
Cost And Copayment Considerations
Even if your insurance covers Zepbound, you may still face certain out-of-pocket costs, such as copayments, coinsurance, and deductibles. Here’s how each can affect you:
- Drug Tier: Medications in higher tiers generally come with higher copays. Zepbound may be a specialty drug, leading to increased copays.
- Out-of-Pocket Maximum: After reaching this amount, insurance should cover further eligible expenses, helping Zepbound users manage long-term costs.
- Deductible: Some plans require meeting a deductible before covering medications, so check if this applies to Zepbound.
Alternative Options If Zepbound Is Denied By Insurance
If Zepbound isn’t covered by your insurance, there are still options to help you manage costs:
- Appeal the Coverage Decision: Many insurance plans allow appeals. Submitting an appeal with supporting information from your doctor can sometimes lead to coverage.
- Explore Patient Assistance Programs: The manufacturer or nonprofit organizations may offer financial assistance for Zepbound.
- Seek Generic Alternatives: While Zepbound may not have an exact generic, similar medications might be available. Discuss alternatives with your healthcare provider.

How To Prepare For Zepbound Prescription Costs Without Insurance
If you are uninsured or if Zepbound isn’t covered, here’s how to manage the financial impact:
- Budget for Monthly Costs: Track the total cost of Zepbound and prepare your monthly budget accordingly.
- Apply for Financial Aid: Many pharmaceutical companies offer aid for high-cost drugs.
- Consider Medical Credit Plans: Some financial institutions offer credit lines specifically for medical expenses, helping you spread out payments.

Frequently Asked Questions About Zepbound Insurance Coverage
Q: Is Zepbound always covered by health insurance?
A: No, Zepbound coverage varies by insurance provider and specific plan.
Q: How can I reduce my out-of-pocket costs for Zepbound?
A: Check if your insurance has a lower copay or coinsurance for Zepbound, consider assistance programs, and reach out to your insurer to confirm if Zepbound is in a lower-cost tier.
Q: What should I do if my insurance denies Zepbound coverage?
A: You can appeal the decision with the help of your healthcare provider and inquire about assistance programs to lower your costs.
Final Thoughts
Securing coverage for Zepbound can be challenging, but by understanding your insurance plan’s formulary, checking for prior authorization, and exploring patient assistance programs, you can potentially reduce out-of-pocket costs. Taking these proactive steps ensures you have the support and guidance to manage your Zepbound prescription effectively.